Learninsta presents the core concepts of Microbiology with high-quality research papers and topical review articles.
Hypersensitivity Types and its Classification
Hypersensitivity is defined as the exaggerated immunological response leading to severe symptoms and even death in a sensitized individual when exposed for the second time. It is commonly termed as allergy. The substances causing allergic/hypersensitivity is known as allergens. Example: Drugs, food stuffs, infectious microorganisms, blood transfusion and contact chemicals.
Classification of Hypersensitivity (Coombs and Gell Classification)
Type I:
Immediate (Atopic or anaphylactic) Hypersensitivity
Type II:
Antibody-dependent Hypersensitivity
Type III:
Immune complex mediated Hypersensitivity
Type IV:
Cell mediated or delayed Hypersensitivity
Type I:
Immediate (Atopic or anaphylactic) Hypersensitivity
This type of hypersensitivity is an allergic reaction provoked by the re-exposure to a specific antigen. The antigen can make its entry through ingestion, inhalation, injection or direct contact. The reaction may involve skin, eyes, nasopharynx and gastrointestinal tract. The reaction is mediated by IgE antibodies (Figure 11.7).
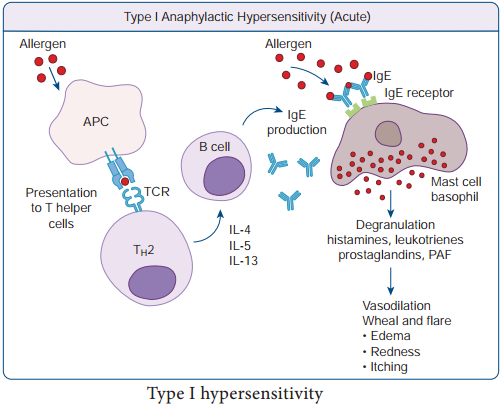
IgE has very high affinity for its receptor on mast cells and basophils. Cross linking of IgE receptor is important in mast cell trigerring. Mast cell degranulation is preceded by increased Ca++ influx.
Basophils and mast cells release pharmacologically active substances such as histamines and tryptase. This causes inflammatory response. The response is immediate (within seconds to minutes). Hence, it is termed as immediate hypersensitivity. The reaction is either local or systemic.
Hay Fever
Allergic rhinitis is commonly known as hay fever. Allergic rhinitis develops when the body’s immune system becomes sensitized and overreacts to something in the environment like pollen grains, strong odour of perfumes, dust etc that typically causes no problem in most people. When a sensitive person inhales an allergen the body’s immune system may react with the symptoms such as sneezing, cough and
puffy swollen eyelids.
Type II Hypersensitivity: Antibody dependent hypersensitivity
In this type of hypersensitivity reactions the antibodies produced by the immune response binds to antigens on the patient’s own cell surfaces. It is also known as cytotoxic hypersensitivity and may affect variety of organs or tissues. Ig G and Ig M antibodies bind to these antigens and form complexes. This inturn activates the classical complement pathway and eliminates the cells presenting the foreign antigen. The reaction takes hours to day (Figure 11.8).
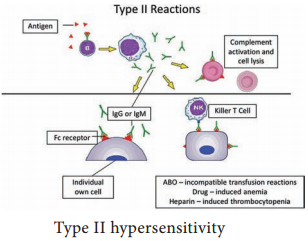
Drug induced haemolytic anaemia Certain drugs such as penicillin, cephalosporin and streptomycin can absorb non-specifically to protein on surface of RBC forming complex similar to hapten-carrier complex. In some patients these complex induce formation of antibodies, which binds to drugs on RBC and induce complement mediated lysis of RBC and thus produce progressive anaemia. This drug induced haemolytic anaemia is an example of Type II hypersensitivity reaction.
Type III Hypersensitivity: Immune complex mediated hypersensitivity
When a huge amount of antigen enters into the body, the body produces higher concentrations of antibodies. These antigens and antibodies combine together to form insoluble complex called immune complex. These complexes are not completely removed by macrophages.
These get attached to minute capillaries of tissues and organs such as kidneys, lung and skin (Figure 11.9). These antigen-antibody complexes activate the classical complement pathway leading to vasodilation. The complement proteins and antigen-antibody complexes attract leucocytes to the area. The leukocytes discharge their killing agents and promote massive inflammation. This can lead to tissue death and haemorrhage.
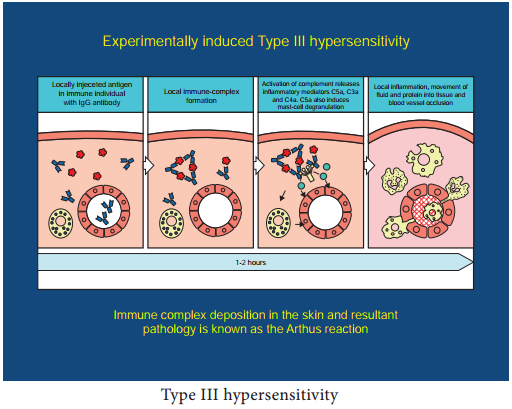
Arthus reaction
It was first observed by Arthus. It is a local immune complex reaction occurring in the skin. Horse serum and egg albumin are the antigens that induce the arthus reaction. It is characterized by erythema, induration, oedema, haemorrhage and necrosis. This reaction occurs when antibody is found in excess. It appears in 2-8 hours after injection and persists for about 12-24 hours (Table 11.1).
Table 11.1: Difference between Immediate Hypersensitivity and Delayed Hypersensitivity
|
Immediate Hypersensitivity |
Delayed Hypersenstivity |
| 1. It appears and disappers rapidly | 1. It appears slowly and last longer. |
| 2. It is induced by antigens or haptens by any route | 2. Induced by infection, injection of antigen intra dermally or with adjuvants of by skin contact. |
| 3. The reaction is antibody mediated B-cell response | 3. The reaction is T-cell mediated response. |
| 4. Passive transfer is possible with serum | 4. Cannot be transferred with serum but can be transferred by lymphocytes |
| 5. Desensitization is easy, but does not last long | 5. Desensitization is difficult but long lasting. |
It is often called as delayed hypersensitivity reaction as the reaction takes two to three days to develop. Type IV hypersensitivity is involved in the pathogenesis of many autoimmune and infectious diseases such as tuberculosis and leprosy. T lymphocytes, monocytes and macrophages are involved in the reaction. Cytotoxic T Cells cause direct damage whereas the T helper cells secrete cytokines and activate monocytes and macrophages and cause the bulk damage (Figure 11.10).
Type IV hypersensitivity: Cell Mediated Delayed Hypersensitivity
Tuberculin reaction (Mantoux Reaction)
When a small dose of tuberculin is injected intra dermally in an individual already having tubercle bacilli, the reaction occurs. It is due to the interaction of sensitized T cell and tubercle bacterium. The reaction is manifested on the skin very late only after 48-72 hours.