Learninsta presents the core concepts of Microbiology with high-quality research papers and topical review articles.
Medical Shigella dysenteriae
The genus Shigellaare exclusively parasites of human intestine and other primates. Shigella dysenteriae is the causative agent of bacillary dysentery or shigellosis in humans. It is a diarrheal illness which is characterized by frequent passage of bloodstained mucopurulent stools.
The four important species of the genus Shigella are: Shigella dysenteriae, Shigella flexneri, Shigella sonnei and Shigella boydii.
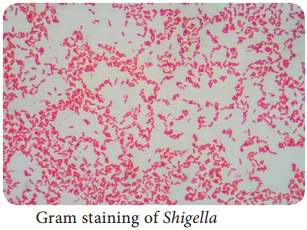
Morphology
Shigella are short, Gram negative rods (0.5µm × 1-3 µm in size). They are non – motile, non – sporing and non – capsulated (Figure 7.12).
Cultural Characteristics
- They are aerobes and facultative anaerobes. Optimum temperature is 37°C and optimum pH – 7.4.
- They can be grown on the following media and show the characteristic colony morphology (Table 7.10 & Figure 7.13)
Table 7.10: Colony morphology of Shigella
|
Media |
Colony Morphology |
| Nutrient Agar | Colonies are circular, convex smooth and translucent |
| MacConkey Agar | Colourless colonies |
| SS – Agar | Colourless colonies |

Toxins
Shigella dysenteriae produces toxins, which is of 3 types, namely, endotoxin, exotoxin and verocytotoxin. The mode of action of these toxins is illustrated in the Table 7.11.
Table 7.11: Various toxins of Shigelladysenteriae
|
Toxins |
Mode of Action |
| Endotoxin | It is released ater autolysis, it has irritating effect on intestinal wall which causes diarrhea and subsequently intestinal ulcers. |
| Exotoxin | It is a powerful toxin and acts as Enterotoxin as well as neurotoxin As Enteroxin – It induces fluid accumulation As Neurotoxin – It damages the endothelial cells of small blood vessels of CNS which results in polyneuritis and coma |
| Vero cytotoxin | It acts on Vero cells |
Pathogenesis
The pathogenic mechanism of Shigella dysenteriaeis discussed below in flowchart 7.5.
Source of Infection – Patient or carriers
Route of entry – faecal – oral route
Site of infection – Large intestine
Incubation Period – Less than 48 hours (1-7 days)
Mode of transmission – Food, finger, faeces and flies
Clinical Manifestations
- Frequent passage of loose, scanty faeces containing blood and mucus.
- Abdominal cramps and tenesmus (straining to defecate).
- Fever and vomiting.
- Hemolytic uremic syndrome (It is a condition caused by the abnormal destruction of red blood cells)
Laboratory Diagnosis
Specimens:
Fresh stool is collected.
Direct Microscopy:
Saline and Lugol’s iodine preparation of faeces show large number of pus cells, and erythrocytes.
Culture:
For inoculation, it is best to use mucus flakes (if present in the specimen) on MacConkey agar and SS agar. After overnight incubation at 37°C, the plates are observed for characteristic colonies, which is confirmed by Grams staining and biochemical reactions.
Treatment and Prevention
- Uncomplicated shigellosis is a self – limiting condition that usually recovers spontaneously.
- In acute cases, oral rehydration therapy (ORT) is done.
- In all severe cases, the choice of antibiotic should be based on the sensitivity of prevailing strain.
- Many strains are sensitive to Nalidixic acid and Norfloxacin.
- Improving personal and environmental sanitation.
- The detection and treatment of patients and carriers.