Learninsta presents the core concepts of Microbiology with high-quality research papers and topical review articles.
Streptococcus pyogenes (Flesh eating Bacteria)
The genus Streptococcus includes a large and varied group of bacteria. They inhabit various sites, notably the upper respiratory tract. However, some species of which Streptococcus pyogenes is the most important and are highly pathogenic. The name Streptococcus is derived from Greek word ‘Streptos’ which means twisted or coiled.
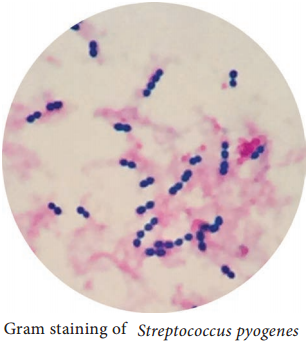
Morphology
- They are Gram positive, spherical or oval cocci and arranged in chains (0.6µm-1µm)
- They are non – motile, non – sporing. Some strains are capsulated (Figure 7.4).
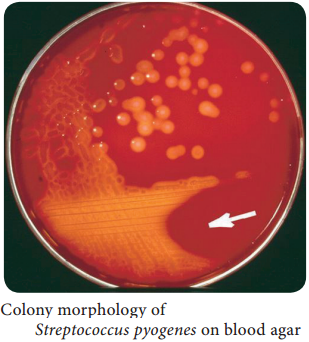
Cultural Characteristics
- They are aerobe and facultative anaerobe. Optimum temperature is 37°C and pH is 7.4 to 7.6
- They grow only in media enriched with blood or serum. It is cultivated on blood agar. On blood agar, the colonies are small, circular, semitransparent, low convex, with an area of clear hemolysis around colonies (Figure 7.5).
- Crystal violet blood agar – a selective medium for Streptococcus pyogenes.
Antigenic Structure
Capsule:
It inhibits phagocytosis
Cell wall:
The outer layer of cell wall consists of protein and lipoteichoic acid which helps in attachment to the host cell. Middle layer of cell wall consists of Group Specific C – Carbohydrate that is used for Lancefield grouping. Inner layer of cell wall is made up of peptidoglycan which has pyrogenic and thrombolytic activity.
Toxins and Enzymes:
Streptococcus pyogenes produces several exotoxins and enzymes which contribute to its virulence.
Toxins and Hemolysins:
Streptococci produces two types of hemolysins which are Streptolysin O and Streptolysin S.
Erythrogenic toxin: (Pyrogenic exotoxin)
The induction of fever is the primary effect of this toxin and it is responsible for the rash of scarlet fever.
Enzymes:
The various enzyme of Streptococcus pyogenes which exhibits virulence activity are listed in Table 7.3.
Enzymes of Streptococcus pyogens and its virulence nature
|
Enzymes |
Virulence nature |
| Streptokinase (fibrinolysin) | It promotes the lysis of human fibrin clot by catalyzing the conversion of plasminogen into plasmin. It facilitates the spread of infection by breaking down the fibrin barrier around the lesions. |
| Deoxyribonucleases | It liquefy the highly viscous DNA that accumulate in thick pusand responsible for thin serous character of streptococcal exudates |
| Hyaluronidase | It breaks down hyaluronic acid of the tissues and favours spread of streptococcal lesion along intercellular spaces. |
| Other enzymes | NADase, lipase, amylase, esterase, phosphates and other enzymes. |
Pathogenesis
Streptococcus pyogenes is intrinsically a much more dangerous pathogen than Staphylococcus aureus and has a much greater tendency to spread in the tissues.
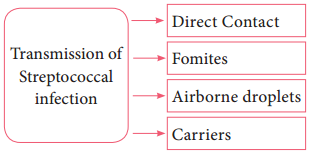
Mode of transmission:
Streptococcal infections are transmitted by the following ways:
Streptococcal diseases may be broadly classified, and it is shown in flowchart 7.1
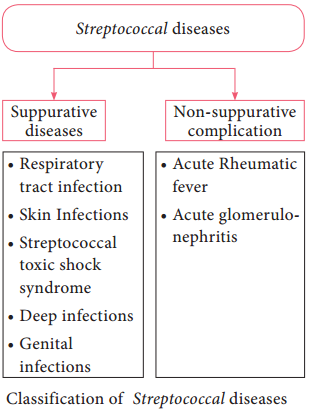
Suppurative Infections
1. Respiratory tract infection
a. Streptococcal sore throat:
Sore throat (acute tonsillitis and pharyngitis) is the most common streptococcal diseases. Tonsillitis is more common in older children and adults. The pathogen may spread from throat to the surrounding tissues leading to suppurative (pus – formation) complication such as cervical adenitis (inflammation of a lymph node in the neck) otitis media (inflammation of middle ear), quinsy (ulcers of tonsils) Ludwig’s angina (purulent inflammation around the sub maxillary glands) mastoiditis (inflammation of mastoid process).
b. Scarlet fever:
The disease consists of combination of sore throat and a generalized erythematous (redness of skin or mucous membranes) rash.
2. Skin infections
a. Erysipeals:
It is an acute spreading lesion. The skin shows massive brawny oedema with erythema it is seen in elderly persons or elders.
b. Impetigo: (Streptococcal pyoderma)
It is a skin infection that occurs most often in young children. It consists of superficial blisters that break down and eroded areas whose surface is covered with pus. It is the main cause leading to acute glomerulonephritis in children.
c. Necrotizing fasciitis:
It is an invasive, infection characterized by inflammation and necrosis of the skin, subcutaneous fat and fascia. It is a life-threatening infection.
3. Streptococcal toxic shock syndrome
Streptococcal pyrogenic exotoxin leads to streptococcal toxic shock syndrome (TSS). It is a condition in which the entire organ system collapses, leading to death.
4. Genital infections
Streptococcus pyogenes is an important cause of puerperal sepsis or child bed fever (infection occur when bacteria infect the uterus following child birth)
5. Deep infection
Streptococcus pyogenes may cause pyaemia (blood poisoning characterized by pus forming pathogens in the blood) septicemia (A condition in which bacteria circulate and actively multiply in the bloodstream) abscess in internal organs such as brain, lung, liver and kidney.
Non – Suppurative Complication
Streptococcus pyogenes infections are sometimes followed by two important non – suppurative complications which are, acute rheumatic fever and acute glomerulonephritis. These complications occur 1-4 weeks after the acute infection and it is believed to be the result of hypersensitivity to some streptococcal
components.
1. Rheumatic fever
It is often preceded by sore throat and most serious complication of haemolytic streptococcal infection. The mechanism by which Streptococci produce rheumatic fever is still not clear. A common cross – reacting antigen exist in some group A streptococci and heart, therefore, antibodies produced in response to the streptococcal infection could cross react with myocardial and heart valve tissue, causing cellular destruction.
2. Acute glomerulonephritis
It is often preceded by the skin infection. It is caused by only a few “nephritogenic types (strains)”. It develops because some components of glomerular basement membrane are antigenically similar to the cell membranes of nephritogenic streptococci.
The antibodies Formed against Streptococci cross react with glomerular basement membrane and damage. Some patients develop chronic glomerulonephritis with ultimate kidney failure.
Laboratory Diagnosis
Specimens:
Clinical specimens are collected according to the site of lesion. Throat swab, pus or blood is obtained for culture and serum for serology.
Direct Microscopy:
Gram stained smears of clinical specimens is done, where Gram positive cocci in chains were observed. It is indicative of streptococcal infection.
Culture:
The clinical specimen is inoculated on blood agar medium and incubated at 37° C for 18-24 hours. After incubation period, blood agar medium was observed for zone of beta – haemolysis around colonies.
Catalase test:
Streptococci are catalase negative which is an important test to differentiate Streptococci from Staphylococci.
Serology:
Serological tests are done for rheumatic fever and glomerulonephritis. It is established by demonstrating high levels of antibody to streptococci toxins. The standard test is antistreptolysin Otitration. ASOtitres higher than 200 units are indicative of prior Streptococcal infection.
Treatment and Prophylaxis
- Penicillin G is the drug of choice.
- In patients allergic to penicillin, erythromycin or cephalexin is used.
- Antibiotics have no effect on established glomerulonephritis and rheumatic fever.
- Prophylaxis is indicated only in the prevention of rheumatic fever, it prevents streptococcal reinjection and further damage to the heart.
- Penicillin is given for a long period in children who have developed early signs of rheumatic fever.