Learninsta presents the core concepts of Biology with high-quality research papers and topical review articles.
Regulation of Kidney Function
ADH and Diabetes Insipidus
The functioning of kidneys is efficiently monitored and regulated by hormonal feedback control mechanism involving the hypothalamus, juxta glomerular apparatus and to a certain extent the heart. Osmoreceptors in the hypothalamus are activated by changes in the blood volume, body fluid volume and ionic concentration.
When there is excessive loss of fluid from the body or when there is an increase in the blood pressure, the osmoreceptors of the hypothalamus respond by stimulating the neurohypophysis to secrete the antidiuretic hormone (ADH) or vasopressin (a positive feedback). ADH facilitates reabsorption of water by increasing the number of aquaporins on the cell surface membrane of the distal convoluted tubule and collecting duct.
This increase in aquaporins causes the movement of water from the lumen into the interstitial cells, thereby preventing excess loss of water by diuresis. When you drink excess amounts of your favourite juice, osmoreceptors of the hypothalamus is no longer stimulated and the release of ADH is suppressed from the neurohypophysis (negative feedback) and the aquaporins of the collecting ducts move into the cytoplasm.
This makes the collecting ducts impermeable to water and the excess fluid flows down the collecting duct without any water loss. Hence dilute urine is produced to maintain the blood volume. Vasopressin secretion is controlled by positive and negative feedback mechanism.
Defects in ADH receptors or inability to secrete ADH leads to a condition called diabetes insipidus, characterized by excessive thirst and excretion of large quantities of dilute urine resulting in dehydration and fall in blood pressure.
Renin Angiotensin
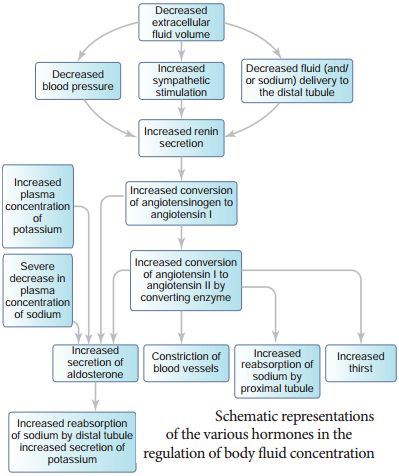
Juxta glomerular apparatus (JGA) is a specialized tissue in the afferent arteriole of the nephron that consists of macula densa and granular cells. The macula densa cells sense distal tubular flow and affect afferent arteriole diameter, whereas the granular cells secrete an enzyme called renin. A fall in glomerular blood flow, glomerular blood pressure and glomerular filtration rate, can atctivate JG cells to release renin which converts a plasma protein, angiotensinogen (synthesized in the liver) to angiotensin I.
Angiotensin converting enzyme (ACE) converts angiotensin I to angiotensin II. Angiotensin II stimulates Na+ reabsorption in the proximal convoluted tubule by vasoconstriction of the blood vessels and increases the glomerular blood pressure.
Angiotensin II acts at different sites such as heart, kidney, brain, adrenal cortex and blood vessels. It stimulates adrenal cortex to secrete aldosterone that causes reabsorption of Na+, K+ excretion and absorption of water from the distal convoluted tubule and collecting duct.
This increases the glomerular blood pressure and glomerular filtration rate. This complex mechanism is generally known as Renin-AngiotensinAldosterone System (RAAS). Figure 8.9 shows the schematic representation of the various hormones in the regulation of body fluid concentration.
Atrial Natriuretic Factor
Excessive stretch of cardiac atrial cells cause an increase in blood flow to the atria of the heart and release Atrial Natriuretic Peptide or factor (ANF) travels to the kidney where it increases Na+ excretion and increases the blood flow to the glomerulus, acting on the afferent glomerular arterioles as a vasodilator or on efferent arterioles as a vasoconstrictor.
It decreases aldosterone release from the adrenal cortex and also decreases release of renin, thereby decreasing angiotensin II. ANF acts antagonistically to the renin – angiotensin system, aldosterone and vasopressin.