Learninsta presents the core concepts of Biology with high-quality research papers and topical review articles.
Disorders of the Circulatory System – Types, Causes and Risk
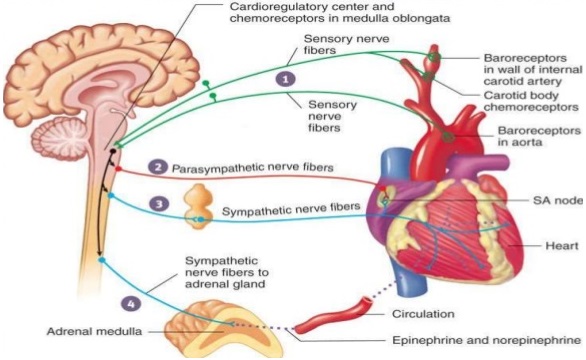
Hypertension
Hypertension is the most common circulatory disease. The normal blood pressure in man is 120/80 mmHg. In cases when the diastolic pressure exceeds 90 mm Hg and the systolic pressure exceeds 150 mm Hg persistently, the condition is called hypertension. Uncontrolled hypertension may damage the heart, brain and kidneys.
Coronary Heart Disease
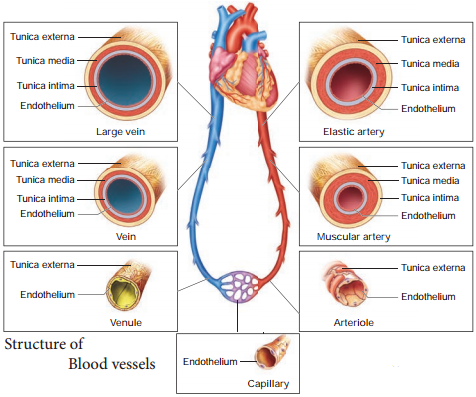
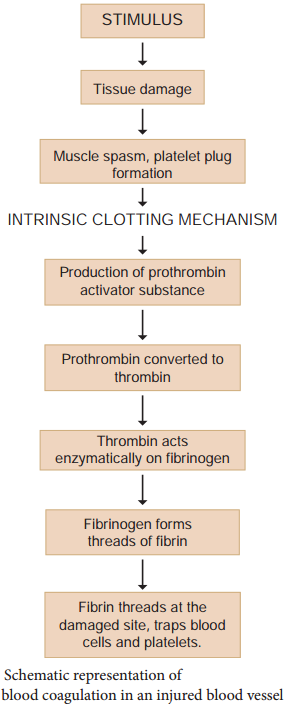
Coronary heart disease occurs when the arteries are lined by atheroma. The build up of atheroma contains cholesterol, fires, dead muscle and platelets and is termed Atherosclerosis. The cholesterol rich atheroma forms plaques in the inner lining of the arteries making them less elastic and reduces the blood flow. Plaque grows within the artery and tends to form blood clots, forming coronary thrombus. Thombus in a coronary artery results in heart attack.
Stroke
Stroke is a condition when the blood vessels in the brain bursts, (Brain haemorrhage) or when there is a block in the artery that supplies the brain, (atherosclerosis) or thrombus. The part of the brain tissue that is supplied by this damaged artery dies due to lack of oxygen (cerebral infarction).
Angina Pectoris
Angina pectoris (ischemic pain in the heart muscles) is experienced during early stages of coronary heart disease. Atheroma may partially block the coronary artery and reduce the blood supply to the heart. As a result, there is tightness or choking with difficulty in breathing. This leads to angina or chest pain. Usually it lasts for a short duration of time.
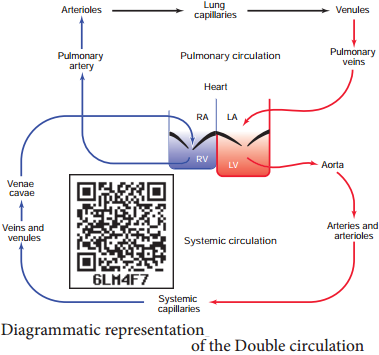
Myocardial Infarction (Heart Failure)
The prime defect in heart failure is a decrease in cardiac muscle contractility. The Frank – Starling curve shifts downwards and towards the right such that for a given EDV, a failing heart pumps out a smaller stroke volume than a normal healthy heart.
When the blood supply to the heart muscle or myocardium is remarkably reduced it leads to death of the muscle fires. This condition is called heart attack or myocardial infarction. The blood clot or thrombosis blocks the blood supply to the heart and weakens the muscle fires.
It is also called Ischemic heart disease due to lack of oxygen supply to the heart muscles. If this persists it leads to chest pain or angina. Prolonged angina leads to death of the heart muscle resulting in heart failure.
Rheumatoid Heart Disease
Rheumatic fever is an autoimmune disease which occurs 2-4 weeks after throat infection usually a streptococcal infection. The antibodies developed to combat the infection cause damage to the heart. Effects include firous nodules on the mitral valve, firosis of the connective tissue and accumulation of fluid in the pericardial cavity.