Learninsta presents the core concepts of Biology with high-quality research papers and topical review articles.
Types of Joints in the Human Body
Types of Joints
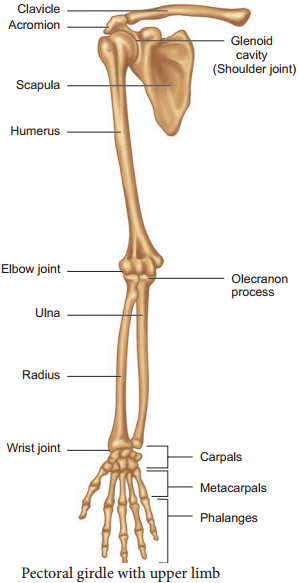
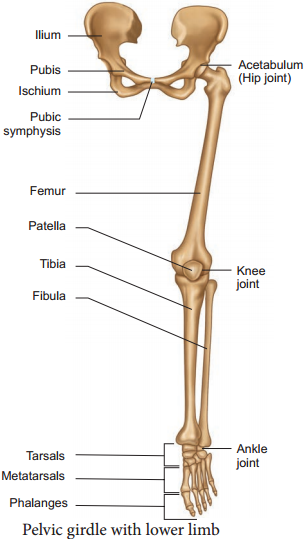
Joints are essential for all types of movements performed by the bony parts of the body. The joints are points of contact (Figure 9.11) between bones. Sometimes they are playing a protective role in the process. Force generated by the muscles are used to carry out the movement through joints which helps human functional activity of daily living and ambulation. The joint acts as a fulcrum of a lever.
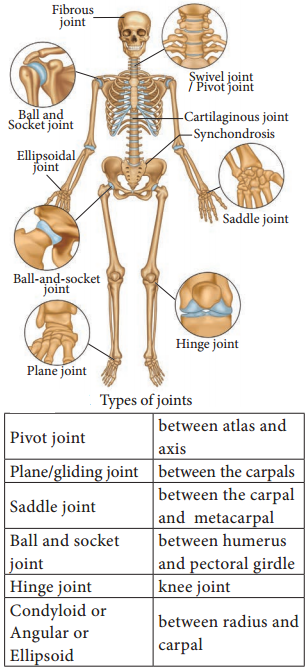
(i) Fibrous Joints or Synarthroses:
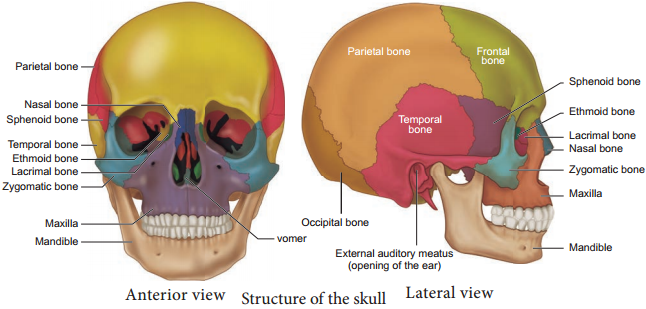
They are immovable field joints in which no movement between the bones is possible. Sutures of the flat skull bones are firous joints.
(ii) Cartilaginous Joints or Amphiarthroses:
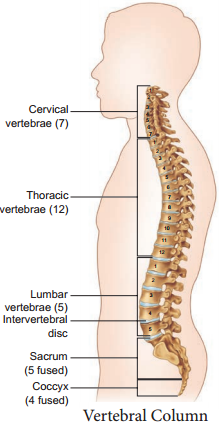
They are slightly movable joints in which the joint surfaces are separated by a cartilage and slight movement is only possible. E.g., Joints of adjacent vertebrae of the vertebral column.
(iii) Synovial Joints or Diarthroses Joints:
They are freely movable joints, the articulating bones are seperated by a cavity which is filled with synovial fluid.
There are six types of freely movable diarthrosis (synovial) joints:
Ball and socket joint. Permitting movement in all directions, the ball and socket joint features the rounded head of one bone sitting in the cup of another bone.
- Hinge joint
- Condyloid joint
- Pivot joint
- Gliding joint
- Saddle joint
There are two basic structural types of joint: diarthrosis, in which fluid is present, and synarthrosis, in which there is no fluid. All the diarthroses (commonly called synovial joints) are permanent. Some of the synarthroses are transient; others are permanent.
With a force strength exceeding 350 kg (772 lbs), the iliofemoral ligament is not only stronger than the two other ligaments of the hip joint, the ischiofemoral and the pubofemoral, but also the strongest ligament in the human body and as such is an important constraint to the hip joint.