Learninsta presents the core concepts of Biology with high-quality research papers and topical review articles.
Role of Other Organs in Excretion
Apart from kidneys, organs such as lungs, liver and skin help to remove wastes. Our lungs remove large quantities of carbon dioxide (18 L/day) and significant quantities of water every day. Liver secretes bile containing substances like, bilirubin and biliverdin, cholesterol, steroid hormones, vitamins and drugs which are excreted out along with the digestive wastes.
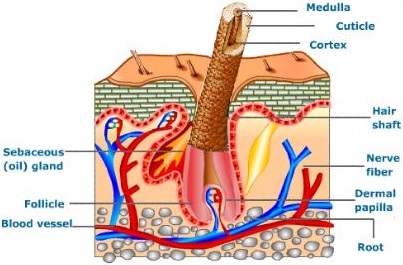
Sweat and sebaceous glands in the skin eliminate certain wastes through their secretions. Sweat produced by the sweat glands primarily helps to cool the body and secondarily excretes Na+ and Cl–, small quantities of urea and lactate.
Sebaceous glands eliminate certain substances like sterols, hydrocarbons and waxes through sebum that provides a protective oily covering for the skin. Small quantities of nitrogenous wastes are also excreted through saliva.
Kidneys play a major role in the process of excretion in humans. Kidneys help in the elimination of wastes from the body in the form of urine. Apart from kidneys, organs like lungs, liver, skin and sebaceous glands help in excretion.
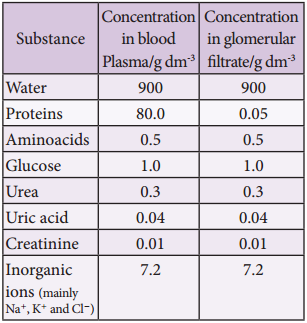
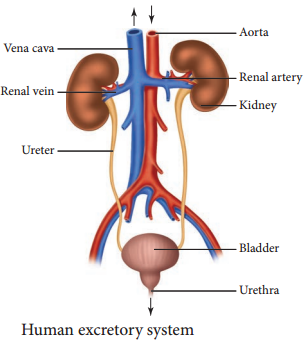
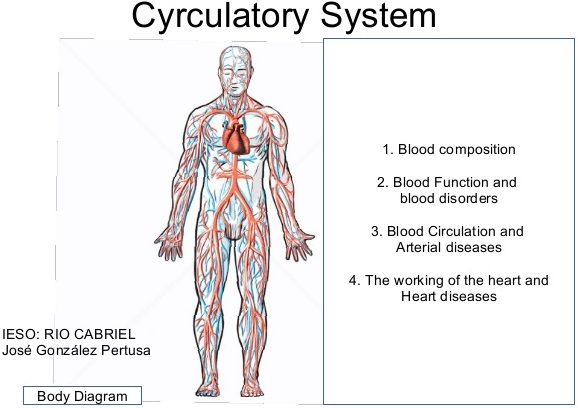
The excretory system in humans consists mainly of the kidneys and bladder. The kidneys filter urea and other waste products from the blood, which are then added to the urine within the bladder. Other organs, such as the liver, process toxins but put their wastes back into the blood.
Excretory Organs. Organs of excretion include the skin, liver, large intestine, lungs, and kidneys (see the figure below). Together, these organs make up the excretory system. They all excrete wastes, but they don’t work together in the same way that organs do in most other body systems. The appendix is a vestigial organ that has no role to play in excretion.
The liver regulates most chemical levels in the blood and excretes a product called bile. This helps carry away waste products from the liver. Production of bile, which helps carry away waste and break down fats in the small intestine during digestion. Production of certain proteins for blood plasma.
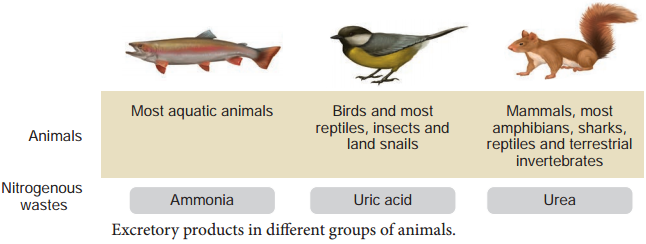
These chemical reactions produce waste products such as carbon dioxide, water, salts, urea and uric acid. Accumulation of these wastes beyond a level inside the body is harmful to the body. The excretory organs remove these wastes. This process of removal of metabolic waste from the body is known as excretion.
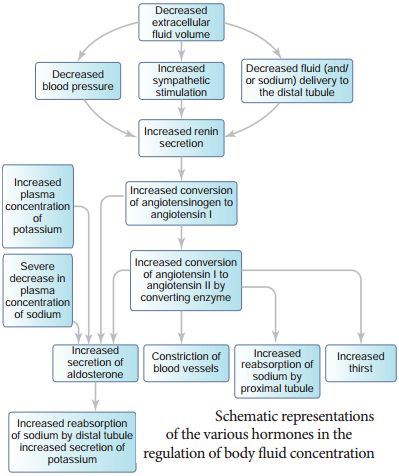
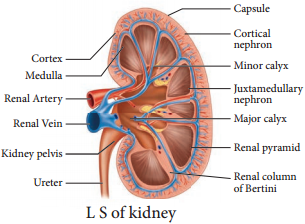
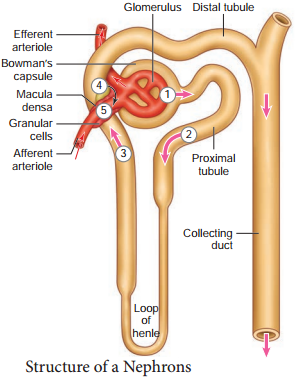
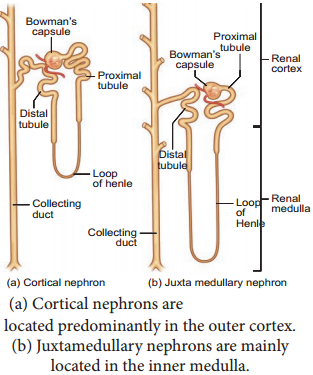
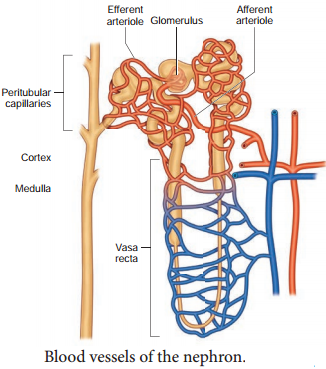
Humans have two kidneys and each kidney is supplied with blood from the renal artery. The kidneys remove from the blood the nitrogenous wastes such as urea, as well as salts and excess water, and excrete them in the form of urine.
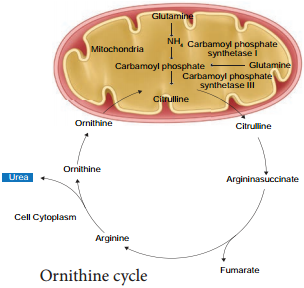
Role of Liver in Excretion:
Liver converts the amino acids present in blood into ammonia and pyruvic acid. Pyruvic acid gets oxidized to release energy and ammonia gets converted into urea. Kidney helps in the filtration of the urea and urea gets excreted in the form of urine.
Certain waste and harmful substances are formed during the functioning of body cells. When these toxic materials are not removed from the body, they get mixed with blood and can damage the cells of the body. The removal of such poisonous waste materials is therefore necessary.
Skin has an important role in excretion in man . So Skin is important to clean our body by the process of excretion. Lungs release Carbon dioxide (CO2) which helps in the process of respiration and purifies blood. Intestine helps in excretion of food digested in stomach and in duodenum.
Excretion, the process by which animals rid themselves of waste products and of the nitrogenous by-products of metabolism. Through excretion organisms control osmotic pressure the balance between inorganic ions and water and maintain acid-base balance.