Learninsta presents the core concepts of Biology with high-quality research papers and topical review articles.
Function of Circulatory Pathways and Its Types
There are two types of circulatory systems, open and closed circulatory systems. Open circulatory system has haemolymph as the circulating fluid and is pumped by the heart, which flows through blood vessels into the sinuses. Sinuses are referred as haemocoel.
Open circulatory system is seen in Arthropods and most Molluscs. In closed circulatory system blood is pumped by the heart and flows through blood vessels. Closed circulating system is seen in Annelids, Cephalopods and Vertebrates.
All vertebrates have muscular chambered heart. Fishes have two chambered heart. The heart in fishes consists of sinus venosus, an atrium, one ventricle and bulbus arteriosus or conus arteriosus. Single circulation is seen in fishes.
Amphibians have two auricles and one ventricle and no inter ventricular septum whereas reptiles except crocodiles have two auricles and one ventricle and an incomplete inter ventricular septum. Thus mixing of oxygenated and deoxygenated blood takes place in the ventricles.
This type of circulation is called incomplete double circulation. The left atrium receives oxygenated blood and the right atrium receives deoxygenated blood. Pulmonary and systemic circuits are seen in Amphibians and Reptiles.
The Crocodiles, Birds and Mammals have two auricles or atrial chambers and two ventricles, the auricles and ventricles are separated by inter auricular septum and inter ventricular septum. Hence there is complete separation of oxygenated blood from the deoxygenated blood. Pulmonary and systemic circuits are evident. This type of circulation is called complete double circulation. The heart, the lungs, and the blood vessels work together to form the circle part of the circulatory system.
3 Kinds of Circulation:
- Systemic circulation
- Systemic Circulation
- Coronary Circulation
- Pulmonary Circulation
- Plasma
The circulatory system consists of three independent systems that work together: the heart (cardiovascular), lungs (pulmonary), and arteries, veins, coronary and portal vessels (systemic).
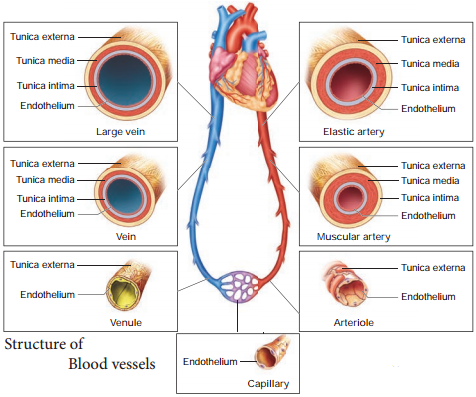
Two main routes for circulation are the pulmonary (to and from the lungs) and the systemic (to and from the body). Pulmonary arteries carry blood from the heart to the lungs. In the lungs gas exchange occurs. Pulmonary veins carry blood from lungs to heart.
Systemic circulation carries oxygenated blood from the left ventricle, through the arteries, to the capillaries in the tissues of the body. From the tissue capillaries, the deoxygenated blood returns through a system of
veins to the right atrium of the heart.
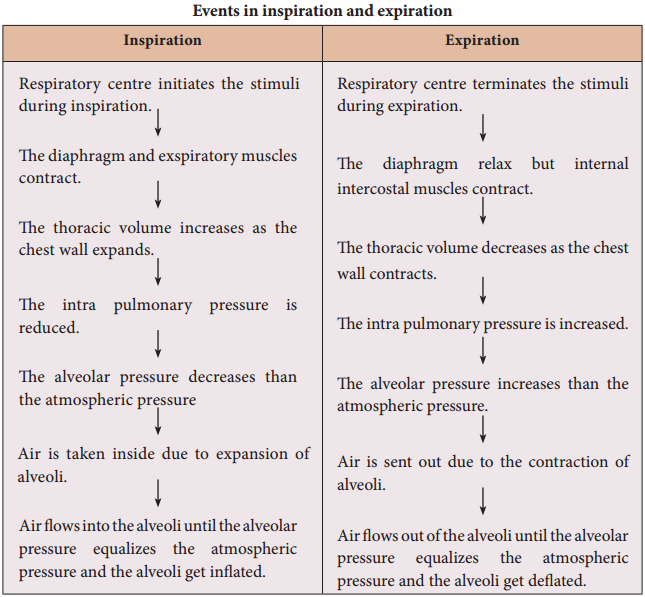
The circulatory and respiratory systems work together to circulate blood and oxygen throughout the body. Air moves in and out of the lungs through the trachea, bronchi, and bronchioles. Blood moves in and out of the lungs through the pulmonary arteries and veins that connect to the heart.